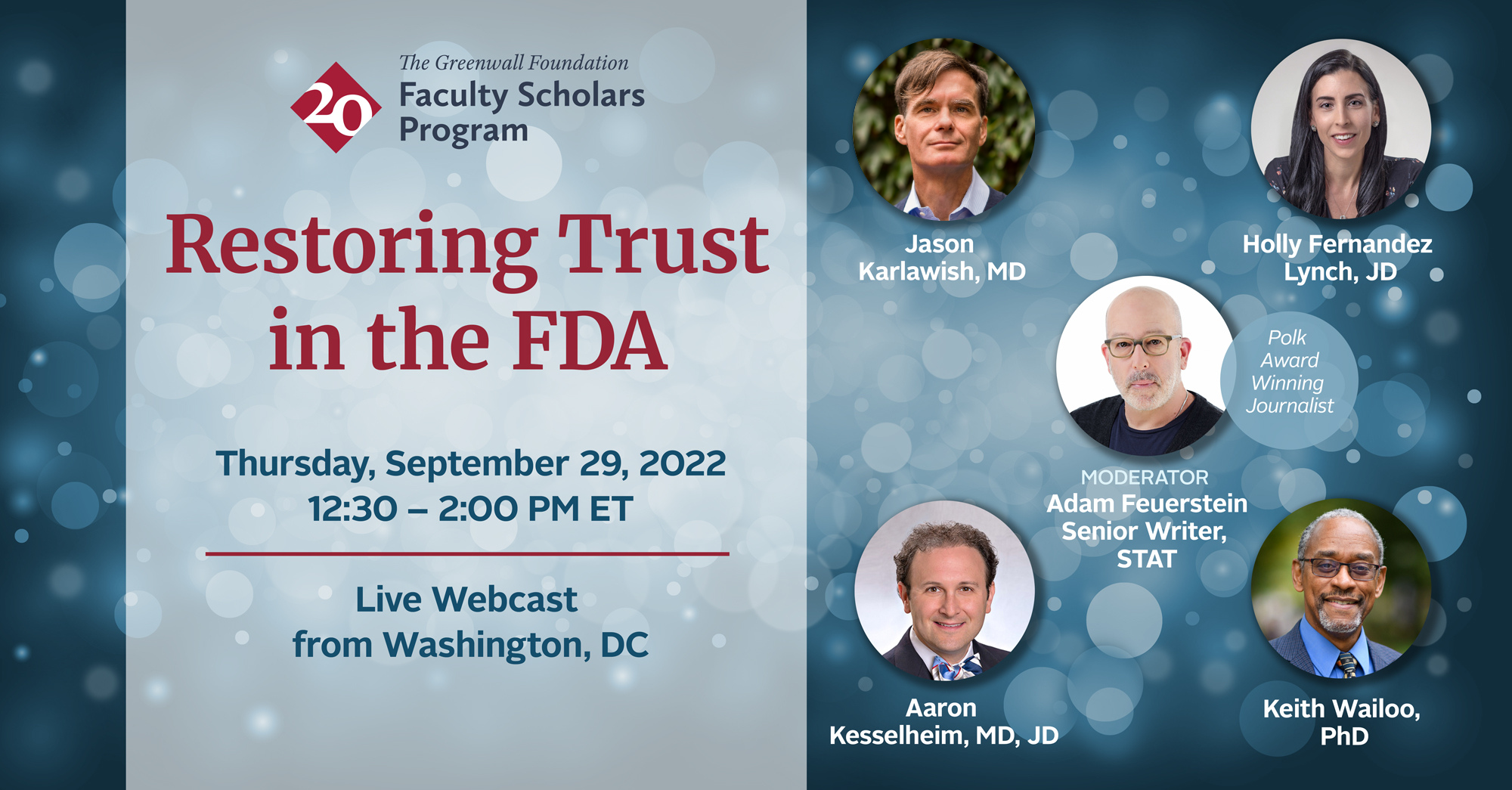
In September, The
Greenwall Foundation hosted a panel
discussion about the state of public trust in the FDA. The participants, which included four members of the Greenwall Faculty Scholars Program community and moderator, journalist Adam Feuerstein, discussed whether and how trust has been lost in the agency, and how it might be won back.
Greenwall Faculty Scholars
and Alums in the audience weighed in with their takes on the discussion on Twitter and here
on our blog. We share some of their reactions below.
Matthew McCoy, PhD
How should FDA interact with patients?
During the panel, Dr. Karlawish raised a critical
question: “How should FDA interact with patients?” Few would dispute that
there’s a role for patient voice in the drug approval process. Patients and
caregivers can offer firsthand accounts of what it’s like to live with a
particular condition and what sorts of treatment options they would value. But
what FDA sometimes refers to as the “patient perspective” is never monolithic.
Different patients have different experiences, different challenges, and
different priorities. It’s therefore important to reflect on how and from whom
FDA solicits patient input. As Dr. Karlawish noted, FDA has issued thoughtful
guidance on collecting representative patient experience data. But many
opportunities for patients to share perspectives directly with the FDA—such as
open public hearings at advisory committee meetings—continue to favor organized
and energized advocates whose views may not reflect those of broader patient
communities. As FDA aims to increase opportunities for patient engagement with
the agency, it should take measures to ensure that it’s capturing a range of patient
perspectives and not being overly reliant on forums that privilege the loudest
voices in the room.
As the panelists rightly noted, FDA
confronts a real challenge when incorporating the patient voice into the drug
approval process generally and into accelerated approval particularly.
Patients with serious diseases who lack meaningful treatment options feel
desperate. And so, it is reasonable that many of them would be willing to
make the tradeoff at the heart of accelerated approval: to sacrifice some
certainty for greater speed.
I would, however, suggest that
there are multiple problems with using patient desperation to justify
acceleration (i.e., accelerated approval). Here are three: (1) Patients
with any given condition are not a monolith despite having the same diagnosis;
for example, some might want to devote resources to care rather than directing
resources to an uncertain, sometimes very expensive, drug while we wait for
results from post-approval trials. FDA needs to better account for these
varied perspectives. (2) The interests of current patients do not
necessarily align with those of future patients who will one day be affected by
the same condition, and FDA has not yet adequately determined how to weigh
future patients’ interests. (3) Listening to patients may not be
enough. The broader public has an interest in the precedents set by
accelerated approval, particularly if an accelerated approval decision will
have follow-on effects for insurance costs (see, e.g., how aducanumab affected
Medicare premiums) or on the level of evidence that suffices for other approval
decisions.
I’ve had the chance to write about
these issues with other Greenwall faculty scholars in the aftermath of
aducanumab’s accelerated approval, and I look forward to continuing to think
about the ethical and policy dimensions.
You can watch watch the panel in its entirety here:

 Lori Freedman, PhD
Lori Freedman, PhD


